Heel Pain

For more information on the heel pain treatments that are available, please use the toggle switches below:

Cracked heels or heel fissures are caused by excessively dry skin. The drier the skin becomes the less elasticity it has causing it to tear into an open wound. It is often described as walking on glass. Most heel fissures are only superficial because the upper layer of the skin known as the epidermis is involved. In severe cases it will affect the next layer of skin or the dermis and this is when fissures become deep and painful.
Skin fissures may appear anywhere on the body but the most common area is around the rim of the heel or other parts of the feet that are exposed to the elements and prone to developing callus.
Working in very wet and damp conditions can also make the skin water logged and this can also cause fissures.
Cracked heels are not harmful unless they become painful or infected.
Fissures are a common foot complaint and can affect a person at any age.
Causes:-
Naturally dry skin i.e hereditary tendency.
Heavy callus
Inflammatory skin conditions like eczema and psoriasis
Low grade fungal infection.
Diabetes and hypothyroidism (under active thyroid).
Exacerbated by:-
Prolonged standing on hard surfaces.
Weight gain
Open foot wear, sandals or flip flops
Climate or environment
Self help for cracked heels :-
Dry cracked heels
Soaking feet in warm water regularly. Dry skin thoroughly and use abrasive foot file to debride rough skin. Then apply a urea based foot balm. This will help to retain some of the moisture after bathing. Foot balms are best applied once or twice daily. Some people find that scraping the hard skin off when the skin is dry is more effective than doing it after a soak. If feet have a low grade fungal infection a broad spectrum anti fungal cream will help.
Wet cracked heels
Expose feet to open air as much as possible. Apply an astringent such as surgical spirit as it helps to dry skin. Wear foot wear and socks made with natural materials if able to.
Severs disease is a condition that causes heel pain and affects children and young adults between the ages of 10-18. Although more common in boys as they tend to have later growth spurts it also happens to girls at an earlier age. Nearly always associated with activity particularly running and jumping. This is because it places the Achilles tendon under enormous stress causing muscle fatigue.
Causes :-
During a child’s growth spurt the soft tissues are unable to keep up with bone growth causing the muscles, tendons and ligaments at the back of the heel to become tight. In fact, the heel is one of the first bones in the body to reach full adult size. The Achilles tendon pulls the bone away from the maturing growth plate during high impact activity causing heel pain.
Symptoms :-
- Pain, swelling & redness in one or both heels
- Tightness & tenderness in the back of the heel – feels worse when squeezed.
- Heel pain increases after running or jumping and feels better after rest
- Difficulty walking
- Walking or running with a limp or on tip toes
The condition can be very disruptive to an individuals quality of life. Sever’s does not cause any long-term foot problems. Symptoms disappear after a few months.
Treatments :-
- Resting or reducing the activity until the pain improves then reintroducing the sports gradually.
- Ice packs
- Stretching exercises
- In severe cases may need a cast so that the heel is forced to rest.
- It can be effectively treated by low level laser therapy, orthotics & advise on appropriate footwear.
Prevention :-
- Supportive shoes
- Stretching exercises
- Warn against over training
- Avoid lots of running on hard surfaces
- Avoid gaining too much weight
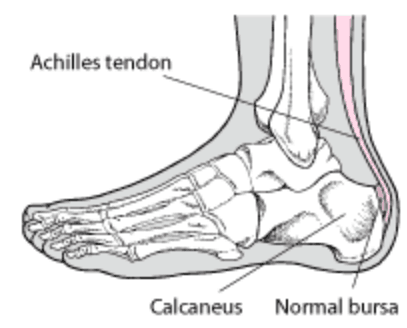
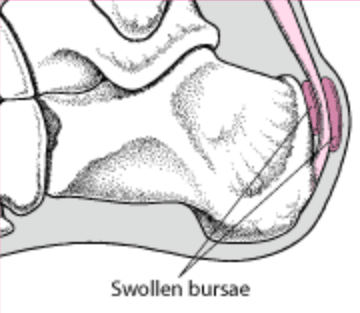
Bursitis is inflammation of the bursa which are small sacs of synovial fluid situated between the bones, tendons and joints. They act as buffers to protect these structures from friction and damage during movement. If a particular body part becomes injured or an infection has developed it can cause inflammation and pain of the affected bursa. The heels are often affected by bursitis.
There are three main types of Bursitis :-
Posterior Achilles tendon bursitis
Occurs mainly in young women who have Haglund’s deformity or ‘pump bumps’ but can develop in men. Walking in high heels or pumps that repeatedly press the soft tissue behind the heel against a stiff shoe counter can cause or aggravate this type pf bursitis.
Posterior Achilles tendon bursitis in the early stage may include redness, pain, and warmth at the back of the heel. If the damage continues the top layer of skin may wear away. After several months, a bursa appears as a soft tender inflamed, red or flesh-coloured nodule. In chronic cases the bursa may become hard like a scar.
Symptoms feel worse when walking, running, standing on tip toes, flexing the foot upwards or when the area is touched.
Retrocalcaneal bursitis
Anterior or deep to the achilles tendon is the retrocalcaneal bursa which may become swollen by any condition that puts extra strain on the Achilles tendon. Injuries to the heel, due to those caused by stiff or poorly fitting shoes and diseases such as rheumatoid arthritis and gout.
Wearing shoes and walking become difficult. A slightly red, swollen tender spot develops on the back of the heel. When the inflamed bursa enlarges, the swelling spreads sideways to both sides of the heel.
Policemans Heel
Policeman’s Heel refers to a protective sack of fluid, know as a bursa, which can form under the plantar tubercle of the heel bone. It is far less common that plantar fasciitis and usually occurs in people with a poor plantar fat pad on the heel.
It is often confused with plantar fasciitis but is not the same. The pain is situated in the middle of the heel pad and is caused by excessive friction and pressure during activity.
Causes :-
- Starting a very intense workout schedule.
- Suddenly increasing activity level without the right conditioning or footwear.
Treatment :-
- Avoid activities that cause pain.
- Warm or cold compress on the heel several times a day.
- Non-steroidal anti-inflammatory medications.
- Protective paddingInsoles/orthotics.
- Low level laser therapy.
- Stretching excercises to improve flexibility and strength around the ankle.
If associated with Achilles tendinitis, you may need to wear a cast on the ankle for several weeks.
Prevention :-
- Wear correct footwear when exercising & walking.
- Exercises to Maintain as good flexibility and strength around the ankle.
If these treatments are not effective, part of the heel bone may need to be surgically removed.
Low Level Laser Therapy has been shown to be very effective in treating this condition reducing the need for pain killing drugs.
A heel spur develops as an irregular growth of the heel bone as calcium deposits are laid down as the plantar fascia pulls away from the heel. Heel spurs can cause extreme pain in the rear of the foot especially when standing or walking.
Causes can be due to biomechanical dysfunction and being overweight as this places the plantar fascia under enormous stress.
Diagnosis is normally from clinical examination or biomechanical assessment and discuss the best course of action to relieve the symptoms. Custom made orthotics are effective in reducing the pain. Treatment aims to reduce the inflammation and identify issues that may be contributing to the problem and advise on the appropriate care plan.
Low Level Laser Therapy is effective in reducing pain.

Haglands bumps are bony enlargements on the posterior aspect of the heel. It is more common in women than men, or in those that have rear foot varus. It is not always painful but can be unsightly. If the bony enlargement is rubbed by foot wear or injured, a small fluid filled sac called a bursa becomes inflamed and a condition called bursitis develops.
Posterior Achilles bursitis is painful and can make walking and wearing certain foot wear difficult. They can appear on one or both feet.
Diagnosis is normally from clinical examination. The Podiatrist is able to assess the factors involved in order to prescribe the necessary corrections to assist recovery.
Causes:-
Haglund’s bumps are genetic but may be also aggravated by the gait of the person who tend to walk on the outer side of the heel.
Signs And Symptoms :-
Pump bumps appear as a noticeable bump on the back of the heel around the Achilles tendon. Swelling and redness may be seen in those who are suffering with pain and this will increase as the inflammation develops and the area becomes more warm and sensitive to the touch.
Treatment :-
- Resting
- Wearing open backed foot wear
- Cold compress several times a day
- Non-steroidal anti inflammatories
- Low level laser therapy
- Padding
- Orthotics to improve gait
- Foot wear wth soft backs
- Shoe modifications
Initially the condition may be treated conservatively as this is less invasive and means the person is less likely to suffer side effects and complications of invasive methods.
Pain relief, rest and ice application may help to reduce the discomfort, redness and swelling of the area which may be enough to ease the condition during flare-ups. Stretching exercises for the Achilles tendon to relieve the pressure of the tissues on the bony structures which in some cases may be sufficient to solve the problem.
For those who have not had any success with less invasive methods or those whose bump protrudes quite significantly surgery may be recommended. Once the surgical correction has taken place the Podiatrist can deal with the Biomechanics to prevent recurrence.
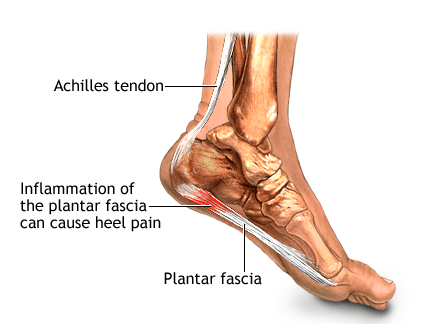
Plantar fasciitis is the most common cause of heel pain. Approximately 2 million patients are treated for this condition every year. It occurs when the strong band of tissue that supports the arch of your foot becomes irritated and inflamed. The plantar fascia is a long, thin ligament that connects the heel to the front of your foot.
Plantar Faciitis can be very painful and can be felt as a dull ache with episodes of a sharp pain in the heel or under the arch. The pain is often worse in the morning or after periods of rest and improves during the day.
Causes :-
The plantar fascia is designed to absorb the high stresses and strains we place on our feet. But, sometimes, too much pressure damages or tears the tissues. The body’s natural response to injury is inflammation, which results in heel pain and stiffness of plantar fasciitis.
In most cases, plantar fasciitis develops without a specific, identifiable reason. There are, however, many factors that can make you more prone to the condition:
- Tight calf muscles that make it difficult to flex your foot
- Weight gain
- Flat feet
- Very high arch
- Repetitive impact activity (running/sports)
- New or increased activity
- Footwear
- Injury
Heel Spurs
Although many people with plantar fasciitis have heel spurs, spurs are not the cause of plantar fasciitis pain.
One in 10 people may have heel spurs, but only 1 in 20 people with heel spurs have foot pain. Because the spur is not the cause of plantar fasciitis, the pain can be treated without removing the spur.

X-ray of heel spur
Diagnosis is normally from patient history and clinical examination, the Podiatrist will discuss the best course of action to relieve symptoms.
Nonsurgical Treatment
Primarily we treat this condition conservatively as this is less invasive and the patient is less likely to suffer side effects and complications than more invasive methods.
90% of patients may improve within 10 months of starting simple treatment methods.
Rest
Decreasing or even stopping the activities that make the pain worse is the first step in reducing the pain. You may need to stop athletic activities where your feet pound on hard surfaces (for example, running or step aerobics).
Ice
Rolling your foot over a cold water bottle or ice for 20 minutes is effective. This can be done 3 to 4 times a day.
Oral Medication
Non-steroidal anti-inflammatory medication such as ibuprofen or naproxen reduce pain and inflammation.
Exercise
Plantar fasciitis is aggravated by tight muscles in your feet and calves. Stretching your calves and plantar fascia is an effective way to relieve the pain.
Orthotics
A biomechanical assessment will provide both static and dynamic information which is then used to fabricate custom made orthotics this will relieve the stress on the plantar fascia.
Low Level Laser
Low level laser therapy is effective in reducing the pain and inflammation and will accelerate the healing.
Other treatments may include night splints or a steriod injection.
For more information click here
Information on running shoes for Plantar Fasciitis click here