Sports Injury

For more information on the sports injury treatments that are available, please use the toggle switches below:

Achilles Tendonitis is inflammation of the tendon caused by micro-tears and results in pain and /or swelling and can affect different areas of the foot and ankle.
The Achilles tendon connects the large calf muscles to the heel bone and provides the power in the lower limb at the ‘push off’ phase of the gait cycle. The Achilles tendon can become inflamed mainly through overuse but there may be other contributory factors. Tendons have a sparse blood supply which is why they are slow to heal.
Achilles tendinitis is not only an injury that affects the sporting community, it can affect any one at any time. However Achilles tendinitis is more common amongst sports people. It often begins with a mild pain after exercise that gradually worsens and stiffens then normally feels better when the tendon warms up. Frequently worse first thing in the morning and after periods of rest so – called ‘start up pain‘.
Causes :-
Sports injury-Muscle fatigue-Overuse and over stretching the tendon beyond its normal limits during sports i.e too much too soon.
Poor Foot Function-Pronation forcing the feet to roll inwards can place an increased strain on the Achilles tendon. As the foot rolls in and the arch flattens the lower leg rotates inwards, which twists and further stresses the Achilles tendon.
Wearing high heels on a regular basis shortens the tendon and when flat shoes are worn, it puts strain on the Achilles tendon causing it to stretch further.
Walking on hard surfaces and up hills.
High arches-tight calf muscles
Some medical conditions
Footwear
Achilles Tendinitis can be acute or chronic
Symptoms :-
Acute
Pain on the achilles tendon during exercise and will gradually come on with prolonged exercise but will go away with rest.
Swelling over the Achilles tendon.
Redness over the skin
Creaking when moving the foot and/or pressing the tendon.
Chronic
Often follows on from acute Achilles tendonitis if the injury is not treated properly or allowed to heal. Chronic Achilles tendonitis is an ongoing problem and can be a difficult condition to treat. The symptoms are similar to those for acute tendonitis, but also include :-
Pain and stiffness in the Achilles tendon, especially in the morning. Diffuse pain along the tendon rather than localised.
Nodules or lumps in the Achilles tendon, particularly 2cm above the heel.
Pain in the tendon when walking – especially up hills or stairs
Low level laser therapy is effective in reducing the pain and inflammation and will accelerate the healing.
For more information click here
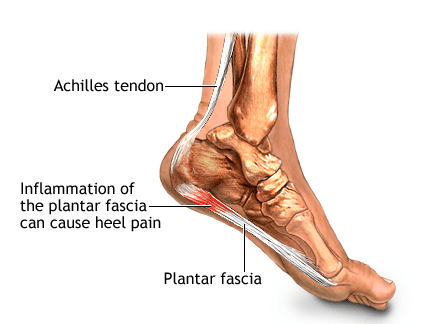
Plantar fasciitis is the most common cause of heel pain. Approximately 2 million patients are treated for this condition every year. It occurs when the strong band of tissue that supports the arch of your foot becomes irritated and inflamed. The plantar fascia is a long, thin ligament that connects the heel to the front of your foot.
Plantar Faciitis can be very painful and can be felt as a dull ache with episodes of a sharp pain in the heel or under the arch. The pain is often worse in the morning or after periods of rest and improves during the day.
Causes :-
The plantar fascia is designed to absorb the high stresses and strains we place on our feet. But, sometimes, too much pressure damages or tears the tissues. The body’s natural response to injury is inflammation, which results in heel pain and stiffness of plantar fasciitis.
In most cases, plantar fasciitis develops without a specific, identifiable reason. There are, however, many factors that can make you more prone to the condition:
- Tight calf muscles that make it difficult to flex your foot
- Weight gain
- Flat feet
- Very high arch
- Repetitive impact activity (running/sports)
- New or increased activity
- Footwear
- Injury
Heel Spurs
Although many people with plantar fasciitis have heel spurs, spurs are not the cause of plantar fasciitis pain.
One in 10 people may have heel spurs, but only 1 in 20 people with heel spurs have foot pain. Because the spur is not the cause of plantar fasciitis, the pain can be treated without removing the spur.

X-ray of heel spur
Diagnosis is normally from patient history and clinical examination, the Podiatrist will discuss the best course of action to relieve symptoms.
Nonsurgical Treatment
Primarily we treat this condition conservatively as this is less invasive and the patient is less likely to suffer side effects and complications than more invasive methods.
90% of patients may improve within 10 months of starting simple treatment methods.
Rest
Decreasing or even stopping the activities that make the pain worse is the first step in reducing the pain. You may need to stop athletic activities where your feet pound on hard surfaces (for example, running or step aerobics).
Ice
Rolling your foot over a cold water bottle or ice for 20 minutes is effective. This can be done 3 to 4 times a day.
Oral Medication
Non-steroidal anti-inflammatory medication such as ibuprofen or naproxen reduce pain and inflammation.
Exercise
Plantar fasciitis is aggravated by tight muscles in your feet and calves. Stretching your calves and plantar fascia is an effective way to relieve the pain.
Orthotics
A biomechanical assessment will provide both static and dynamic information which is then used to fabricate custom made orthotics this will relieve the stress on the plantar fascia.
Low Level Laser
Low level laser therapy is effective in reducing the pain and inflammation and will accelerate the healing.
Other treatments may include night splints or a steriod injection.
For more information click here
Foot fractures can range from a slight crack in the bone to a complete break that goes through the skin. Pain is worse when standing or walking.
Treatment depends on the location and type of injury. Diagnosis is usually from clinical examination and x-rays The Podiatrist is able to assess the factors involved in order to prescribe the necessary corrections to assist recovery.
Severs disease is a condition that causes heel pain and affects children and young adults between the ages of 10-18. Although more common in boys as they tend to have later growth spurts it also happens to girls at an earlier age. Nearly always associated with activity particularly running and jumping. This is because it places the Achilles tendon under enormous stress causing muscle fatigue.
Causes :-
During a child’s growth spurt the soft tissues are unable to keep up with bone growth causing the muscles, tendons and ligaments at the back of the heel to become tight. In fact, the heel is one of the first bones in the body to reach full adult size. The Achilles tendon pulls the bone away from the maturing growth plate during high impact activity causing heel pain.
Symptoms :-
- Pain, swelling & redness in one or both heels
- Tightness & tenderness in the back of the heel – feels worse when squeezed.
- Heel pain increases after running or jumping and feels better after rest
- Difficulty walking
- Walking or running with a limp or on tip toes
The condition can be very disruptive to an individuals quality of life. Sever’s does not cause any long-term foot problems. Symptoms disappear after a few months.
Treatments :-
- Resting or reducing the activity until the pain improves then reintroducing the sports gradually.
- Ice packs
- Stretching exercises
- In severe cases may need a cast so that the heel is forced to rest.
- It can be effectively treated by low level laser therapy, orthotics & advise on appropriate footwear.
Prevention :-
- Supportive shoes
- Stretching exercises
- Warn against over training
- Avoid lots of running on hard surfaces
- Avoid gaining too much weight
Achilles Tendonitis ( degeneration / inflammation )
Achilles Tendon Rupture
Shin splints or medial tibial stress syndrome refers to pain along the inner border of the shinbone (tibia). They develop during and after exercise and more common with running or vigorous sports activity. Taking care not to overdo your activities will help prevent shin splints.
Shin splints are inflammation of the muscles, tendons, and bone tissue around your tibia. Pain occurs along the inner border of the shin bone down the front of the lower legs where the muscles attach to bone.
Although shin splints are not serious, the pain can stop you from exercising and may get worse. It’s important not to run through the pain.
Symptoms :-
- Starts soon after exercise
- Pain gradually improves when resting and sometimes fades while still exercising, but it can eventually become constant and continue even when resting
- Pain is dull and achy at first, but may become increasingly sharp or severe and stop you exercising
- Can affect one or both shins
- Pain is generalised over a large area the shin unlike a fracture which is localised
- There may be swelling
Causes :-
- Brought on by running or repetitive weight bearing on the legs. It’s thought this leads to swelling (inflammation) of the tissue around the shin bone.
- Several things can increase your chances of getting shin splints, including :-
- Sudden change in activity levels
- Running on hard or uneven surfaces
- Poorly fitting or worn-out trainers.
- Weight gain
- Flat feet (pronation)
- Very high arches (supination)
- Tight calf muscles & Achilles tendon & ankle instability
In general, shin splints develop when the muscle and bone tissue (periosteum) in the leg become overworked by repetitive activity.
Shin splints often occur after sudden changes in physical activity. These can be changes in frequency, such as increasing the number of days you exercise each week. Changes in duration and intensity, such as running longer distances or on hills, can also cause shin splints.
Treatment :-
- Rest – standard treatment includes several weeks of rest from the activity that caused the pain.
- Ice pack on painful area for around 10 minutes several times a day for the first few days. Do not apply ice directly to the skin.
- Pain killers – ibuprofen, aspirin, and naproxen reduce pain and swelling.
- Low impact exercises until shin splints improve, such as swimming, using a stationary bike, or an elliptical trainer.
- Compression – elastic compression bandage may prevent additional swelling.
- Orthotics – from a podiatrist particularly people who have flat feet
Shin splints usually resolve with rest and the simple treatments described above.
Prevention :-
- Wear appropriate trainers for activity
- Run on softer flatter surfaces (recreation ground or playing field)
- Introduce changes to your activity gradually
- Mix high-impact exercises with low-impact exercises
- Maintain a healthy weight
- Improve strength & flexibility
- Warm up and stretch thoroughly before & after exercises.
Low level laser therapy helps to reduce swelling & pain and accelerate repair of damaged tissue.
The immediate pain-relieving effects, which can occur within minutes of application, are brought about by three responses :-
- Neural blockage in peripheral and sympathetic nerves, particularly nociceptors. (blocks nerve pain)
- Reduction of muscle spasm.
- Improvement in local oedema, especially in acute injury. (reduces swelling)
Influencing all three phases of wound healing: the inflammatory, proliferative and remodelling phases, photobiomodulation promotes ATP synthesis, induces cell proliferation, accelerates collagen synthesis, increases tensile strength and influences the concentration of prostaglandins thus reducing pain associated with inflammation.
As symptoms improve you can slowly build up your fitness level to strengthen the muscles and improve range of motion and balance.

Freiberg’s Infraction occurs when the head of the second (and sometimes the third and fourth) metatarsal bones have a loss of blood supply. Most commonly amongst children 10 – 17 years of age.
Caused by stress or injury to the foot along with sporting activities and rapid skeletal growth.
Diagnosis is normally from clinical examination or biomechanical assessment in addition to discussing the best course of action to relieve the pressure on the metatarsal head. LLLT has been effective in healing the damaged tissues and orthotics may be recommended.
Achilles Tendon Rupture is a serious injury which needs to be diagnosed and treated as soon as possible. The Achilles tendon joins the heel bone to the calf muscles and its function is to flex the foot at the ankle. If the Achilles tendon is torn, the tear may be either partial or complete. In a partial tear, the tendon is partly torn but still joined to the calf muscle. With complete tears, the tendon is completely torn so that the connection between the calf muscles and the heel bone is lost.
Ruptures occur through a sudden contraction of the calf muscle and is commonly linked with racquet sports (Squash, Badminton, Tennis) but can occur as a result of a fall or stumble. It can occur at any age but is most common in people between the ages of 30 and 50.
Causes:-
- Any muscle or tendon in the body can be torn if there is excessive stress placed on it.
- High impact sports, football, running, basketball, diving and tennis.
- Falls forcing the foot upwards and stretching & tearing the tendon.
- A deep cut in the tendon.
- Long-term use of Corticosteroids.
- Steroid injections near Achilles tendon.
- Cushing’s syndrome.
- A weak Achilles tendon from a previous sprain.
- Rheumatoid arthritis, gout and lupus.
Symptoms :-
- Comes on suddenly during a sporting activity or injury.
- You might hear a snap or feel a sudden sharp pain when the tendon is torn.
- The sharp pain usually settles quickly, although there may be some aching at the back of the lower leg.
- After the injury, the usual symptoms are :-
- A flat-footed type of walk.
- You can walk and bear weight but cannot push off the ground properly on the side where the tendon is ruptured.
- Unable to stand on tiptoe. If the tendon is completely torn, you may feel a gap just above the back of the heel.
- However, if there is bruising then the swelling may disguise the gap.
Diagnosis :-
Achilles tendon rupture is often misdiagnosed as a sprain, however an experienced Podiatrist will make a diagnosis from clinical examination and the history of the injury. A method known as the calf squeeze test may be used. The podiatrist will gently squeeze the muscle at the back of your leg and observe how the ankle moves (plantar flexion). This is an accurate test for Achilles Tendon Rupture.
Treatment :-
Non-surgical management traditionally was selected for minor ruptures, less active patients, and those with medical conditions that prevent them from undergoing surgery.
Low level laser therapy is effective in reducing the pain and inflammation and will accelerate the healing and help prevent the formation of scar tissue. None operative treatment is associated with a higher re-rupture rate however this is less invasive and the patient is less likely to suffer side effects and complications than more invasive methods.
If conservative methods fail surgery may be required. The period of immobilisation after surgery is about eight weeks and it takes about six months to return to normal activity. Treatment involves wearing a plaster cast or brace (orthosis) for several weeks, and possibly having an operation. Recent studies have produced superior results with much more rapid rehabilitation in fixed or hinged boots.
Low level laser therapy also referred to as ‘pure light therapy’ speeds up the body’s natural healing process in damaged tissues by energising the biochemical responses within our cells.
LLLT also stimulates the release of our body’s natural painkillers known as endorphins and provides a rapid and effective form of pain relief and may eliminate the need for painkilling drugs. It accelerates repair in acute injuries as well as stimulates and optimises the body’s natural healing process through controlled application of specific wavelengths of light which have particular physiological effects.
Because the effects of LLLT are biochemical and not thermal it cannot cause heating and damage to living tissue. It is therefore a safe and painless, drug-free, non-invasive method of treatment.
LLLT is used in the treatment of:-
- Pain Relief – Rheumatoid Arthritis, Osteo Arthritis, Heel Pain, Metatarsalgia, Plantar Fasciitis, Morton’s Neuroma, Sprains and Strains.
- Sports Medicine – injuries related to sports activities.
- Skin Conditions – Verrucae (efficient and pain free – ideal for children), warts, eczema.
- Wound Healing – Foot Ulcers, Diabetic, Venus Ulcers, Neuropathic Ulcers, Ischaemic Ulcers and Soft Tissue Repair.
For more information about Low Level Laser Therapy click here

Orthotics are specialized insole devices that correct or modify how the foot functions. They keep the foot properly aligned and can redistribute the weight placed on the foot to change its function, protect the foot, or both.
When the foot is not functioning correctly, painful areas result. Appropriately prescribed orthotics can help solve a number of biomechanical related problems hence reduce pain, not only in the foot. They can also reduce pain in other parts of the body such as the knee, hip and lower back. They can also increase stability in an unstable joint and prevent a deformed foot from developing additional problems and improve overall quality of life.
Depending on the problem orthotics range from a simple insole to offload painful corns and callus to a semi bespoke over the counter device to a bespoke custom made orthotic.
Over the counter orthotics
Over the counter orthotics are available and can help people with minor symptoms however they cannot correct a wide range of symptoms.
Custom made orthotics
The most effective are custom made orthotics in which a mould is made of your foot so that the orthotics work precisely with your uniquely individual foot structure. The orthotics are specially created in a laboratory to correct misalignments and deformities so that when they are placed in your shoes your feet are perfectly aligned.
Different types of material are used to construct custom made orthotics depending upon the patients needs.
Rigid orthotics
Rigid orthotics are designed to control function and are mainly used for walking or dress shoes. They control motion in the two major foot joints that lie directly below the ankle joint and are usually made of a firm material such as plastic or carbon fibre. They are designed to improve or eliminate strains, aches and pains in the legs, thighs and lower back.
Soft orthotics
Soft orthotics help absorb shock, increase balance and take pressure off painful areas. They are effective for patients with diabetes, arthritis, or deformed feet. Soft custom made orthotics are usually made of soft, cushioned materials so that they can be worn against the sole of the foot, extending from the heel past the ball of the foot together with the toes and will protect the feet from stress.
Semi-rigid orthotics
Semi-rigid orthotics help correct foot balance for walking or participating in sports. They are typically made of layers of soft material reinforced with rigid materials for support. They are often used by athletes to reduce pain when they train and compete.
Capsulitis typically linked with acute trauma (sports injury or over use) the area becomes hot swollen and painful.
Diagnosis is made from clinical examination and biomechanical assessment. LLLT has been shown to be very effective in treating this condition reducing the need for painkilling drugs. Orthotics may be recommended if there is an underlying biomechanical problem.