Low Level Laser Therapy
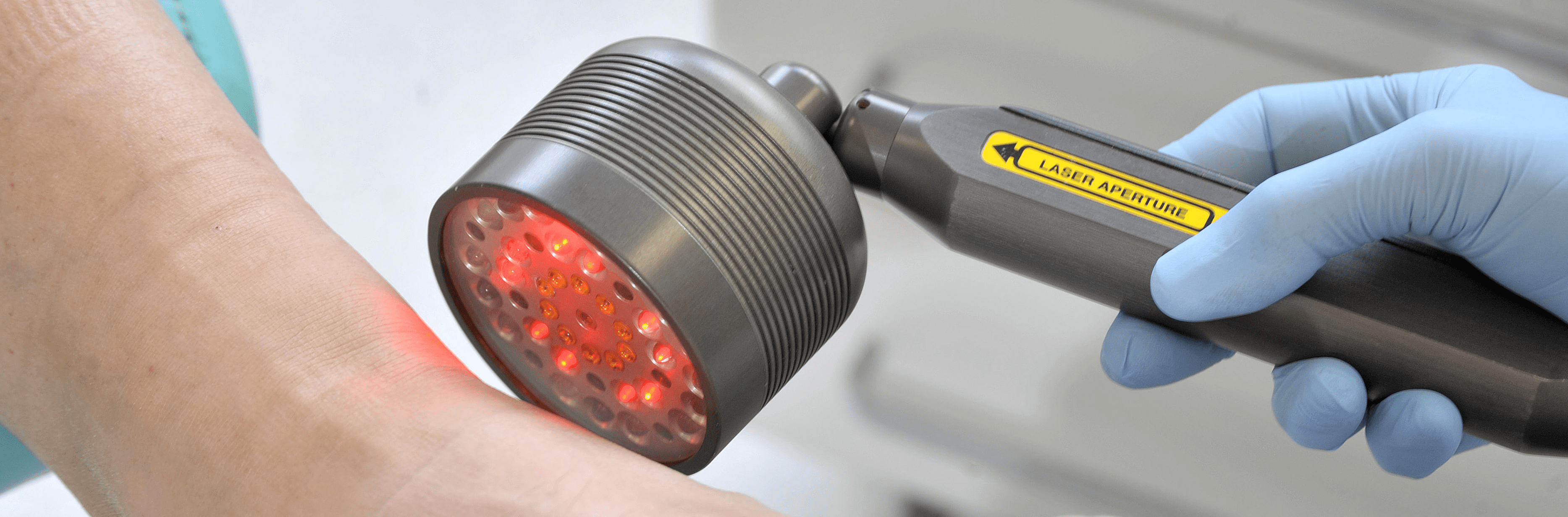
Low level laser therapy also referred to as ‘pure light therapy’ accelerates the body’s natural healing process by energising the biochemical responses within our cells.
Often called ‘soft’ laser, the laser beam does not cut or burn and has no side effects, other than the feeling of relaxation, therefore cannot cause heating, pain or damage to living tissue. LLLT also stimulates the release of our body’s natural painkillers ‘endorphins’ and provides a rapid effective form of pain relief that may eliminate the need for painkilling drugs. It is therefore a safe and painless, drug-free, non-invasive method of treatment.
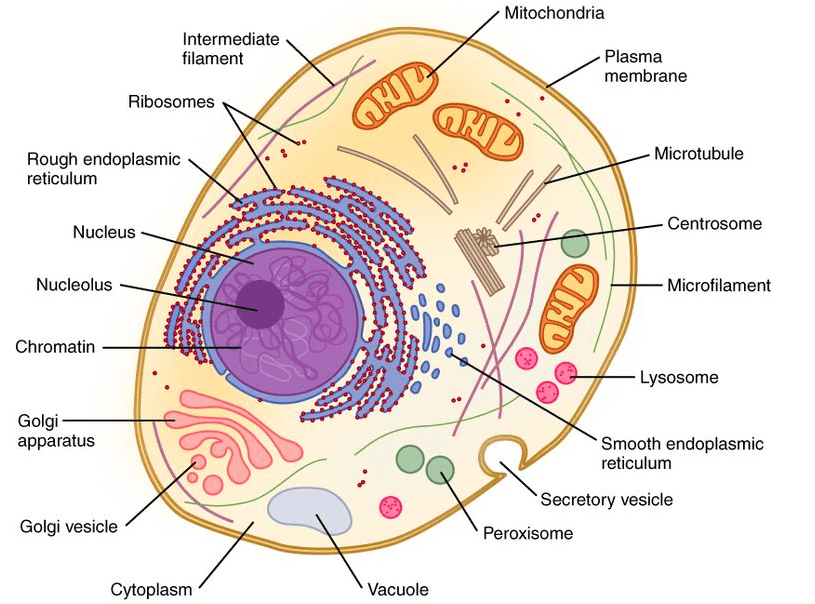
Particular wavelengths of light stimulate the body’s healing cells: initial absorption by the mitochondria leads to increased fibroblast cell proliferation and migration, with modulation of cytokine levels, growth factors, inflammatory mediators and increased tissue oxygenation – all part of the natural healing process.
Essentially by directly treating the damaged tissue with appropriate light, laser therapy helps the body to heal itself. It is especially effective for chronic conditions, or where the immune system is compromised, as it can also re-start a stalled healing process.
In addition to the local cellular effects, research on low level laser therapy has demonstrated both enhanced levels of endorphin release, and the suppression of pain messages previously sent to the brain.
It has been used for over 30 years and is widely available in the medical field for treatment of pain, wound healing and musculoskeletal conditions.
Treatment is quick, pain-free, easy to apply and effective.
Patients respond quickly when treating soft tissue conditions and pain, with results usually evident in the first 1-2 treatments, other conditions vary.
LLLT is successfully used in the treatment of:-
- Pain Relief – Plantar Fasciitis, Heel Pain, Metatarsalgia, Bursitis, Morton’s Neuroma, Sprains, Strains, tendinopathies, Rheumatoid Arthritis, Osteo Arthritis, and neuropathy
- Fungal Nails – successful treatment of fungal nails.
- Verrucae – (efficient and pain free – ideal for children), warts.
- Sports Medicine – injuries related to sports activities.
- Skin Conditions – eczema and psoriasis
- Wound Healing – Foot Ulcers, Diabetic, Venous Ulcers, Neuropathic Ulcers, Ischaemic Ulcers, chilblains, post surgical wounds and burns.
- Bone Repair – has been shown to improve bone repair treating fractures.
- Scar tissue-Pre-existing scar tissue has shown improvement after laser treatment.
For more information on the low level laser therapy treatments that are available, please use the toggle switches below:

Gout is a condition caused by abnormally high levels of uric acid in the blood.
The large toe joint in the foot is commonly affected. Crystals accumulate around the joint causing acute inflammation and intense pain. The initial attack is usually the worst as the onset is sudden and often comes on at night.
Repeated attacks of gout can cause arthritis in the affected joints if left untreated.
Symptoms:-
Sudden attack of severe pain in one or more joints.
Joint feeling hot and tender, unable to bear anything coming into contact with it.
Swelling.
Red shiny skin over affected joint.
Peeling, itching and flaking skin as swelling subsides.
Treatments:-
Take medication prescribed by your G.P. as soon as you notice an attack.
Rest and elevate the limb.
Keep the joint cool by applying ice packs for no more than 20 minutes keeping the ice pack wrapped in a towel, otherwise this can damage the skin.
Keep well hydrated, this will help flush out the crystals.
Low Level Laser Therapy has proven to be successful in treating gout in the early stages.

Onychomycosis is a fungal infection that occurs as a result of the fungi that cause athletes foot infecting either the fingernails or toenails. Usually spreading from the skin into the nails. The most prevalent fungi that infects the foot is called a “dermatophyte”. Fungal infections normally develop over time, so any immediate difference may not cause any obvious signs at first.
Symptoms :-
Fungal toe nails often appear to have white yellow or brown patches and may alter in its structure. It can affect a small part of the toe nail or the whole the nail sometimes making it thick crumbly and brittle and very difficult to cut.
As it progresses, the infection can cause :-
- Discolouration of the nail – it may turn white, black, yellow or green
- Thickening and distortion of the nail – it may become an unusual shape and be difficult to trim
- Pain or discomfort – when placing pressure on the affected nails
- Pieces may crumble, break off and come away completely
- The surrounding skin may also become infected and become itchy, flaky dry or red and swollen.

Causes :-
- You’re more liable to get a fungal nail infection if you:-
- Don’t keep your feet clean and dry
- Hot and sweaty feet
- Wear shoes made of man made materials
- Walking barefoot in communal showers, gyms and changing rooms is where most people catch fungal infections
- Injuries
- A weak immune system
- Diabetes, psoriasis, obesity or peripheral arterial disease
- Living in hot and humid climates.
- Severe injuries to the nail may also lead to a bacterial infection
Communal areas where there are showers changing rooms and gyms are where people are most likely to come in to contact with this type of infection. If you get a manicure or pedicure at a nail salon, be sure to ask how the staff disinfects their tools and how often they do it. Tools, such as emery boards and nail clippers, can spread fungal infections from person-to-person if they’re not sanitized.
Prevention:-
You can reduce your risk of developing a fungal nail infection by:-
- Keeping your hands and feet clean and dry
- Well-fitting shoes and clean socks made of natural materials
- Keeping the nails short
- Using your own clippers and towels and not sharing with other people
- Wearing flip flops or protective shower shoes in communal areas
- Replacing infected footwear or have them sanitised
- Treat athletes foot as soon as possible to prevent the infection spreading to your nails
- Nail salon equipment can sometimes be the source of fungal nail infections. If you regularly visit a salon, make sure any equipment used is properly sterilised between uses.
- Fungal nail infections can be spread to other people, so you should take steps to avoid this if you have an infection.


Treatments :-
- Oral anti fungal medication (possible side effects)
- Nail Laquer (we have not found this to be very successful)
- A procedure to remove the nail completely may be recommended in severe cases
- Low level laser treatment, where a high-energy laser is used to destroy the fungus.(no side effects)
Treatment or not, you should still practise good foot hygiene to stop the infection getting worse or spreading to others.
A Podiatrist will be able to diagnose fungal nails and advise on the appropriate care plan.
At Market Street Clinic we have Low Level Laser therapy for the successful treatment of fungal nails and a UV shoe steriliser to clean and deodorises shoes with UV lights for disinfecting shoes.
Treated with two different Laser probes, a special probe to treat the newly exposed surface, then the infected nails with a penetrative probe of invisible light. This treatment is completely pain free and safe there is no pain or burning of skin or nail, so there is no recovery period or detrimental effect on activity after treatment.
Has major benefits over topical and the risks of oral medication which include effectiveness and side effects.
Following treatment you will be required to topically medicate the treated nails to protect them from further infection until your follow up appointment. Photographs are taken for comparative purposes and monitoring of your results. Preventative advice is given and your footwear can be sanitised using our UV light machine. All of our equipment is sterile.
An effective treatment for restoring fungal infected and thickened discoloured nails.
Daily Mail article on Low level laser therapy link:-
http://www.dailymail.co.uk/health/article-2110800/Pain-free-laser-banishes-toenail-fungus.html
Results of gov clinical trials on Low level laser therapy :-
https://clinicaltrials.gov/ct2/show/NCT01534689
Market Street Clinic Low Level Laser Therapy treatment results






2 before and after
3 before and after
When you go for your laser nail treatment, be sure to bring clean socks to wear after your laser toenail treatment and ask for the shoes too be sanitized. That way your newly treated toenails will go back in a healthy, germ-free shoe.

Achilles Tendinitis is inflammation of the tendon caused by micro-tears and results in pain and /or swelling and can affect different areas of the foot and ankle.
The Achilles tendon connects the large calf muscles to the heel bone and provides the power in the lower limb at the ‘push off’ phase of the gait cycle. The Achilles tendon can become inflamed mainly through overuse but there may be other contributory factors. Tendons have a sparse blood supply which is why they are slow to heal.
Achilles tendinitis is not only an injury that affects the sporting community, it can affect any one at any time. However Achilles tendinitis is more common amongst sports people. It often begins with a mild pain after exercise that gradually worsens and stiffens then normally feels better when the tendon warms up. Frequently worse first thing in the morning and after periods of rest so – called ‘start up pain‘.
Causes :-
Sports injury-Muscle fatigue-Overuse and over stretching the tendon beyond its normal limits during sports i.e too much too soon.
Poor Foot Function-Pronation forcing the feet to roll inwards can place an increased strain on the Achilles tendon. As the foot rolls in and the arch flattens the lower leg rotates inwards, which twists and further stresses the Achilles tendon.
Wearing high heels on a regular basis shortens the tendon and when flat shoes are worn, it puts strain on the Achilles tendon causing it to stretch further.
Walking on hard surfaces and up hills.
High arches-tight calf muscles
Some medical conditions
Footwear
Achilles Tendinitis can be acute or chronic
Symptoms :-
Acute
Pain on the achilles tendon during exercise and will gradually come on with prolonged exercise but will go away with rest.
Swelling over the Achilles tendon.
Redness over the skin
Creaking when moving the foot and/or pressing the tendon.
Chronic
Often follows on from acute Achilles tendinitis if the injury is not treated properly or allowed to heal. Chronic Achilles tendinitis is an ongoing problem and can be a difficult condition to treat. The symptoms are similar to those for acute tendonitis, but also include :-
Pain and stiffness in the Achilles tendon, especially in the morning. Diffuse pain along the tendon rather than localised.
Nodules or lumps in the Achilles tendon, particularly 2cm above the heel.
Pain in the tendon when walking – especially up hills or stairs
Low level laser therapy is effective in reducing the pain and inflammation and will accelerate the healing.
Treatment would involve the lower calf muscle area plus any tender trigger points being treated every other day for a couple of weeks. Helpful muscle relaxation is best achieved by applying the laser to relevant acupuncture points.
For more information click here
Achilles Tendon Rupture is a serious injury which needs to be diagnosed and treated as soon as possible. The Achilles tendon joins the heel bone to the calf muscles and its function is to flex the foot at the ankle. If the Achilles tendon is torn, the tear may be either partial or complete. In a partial tear, the tendon is partly torn but still joined to the calf muscle. With complete tears, the tendon is completely torn so that the connection between the calf muscles and the heel bone is lost.
Ruptures occur through a sudden contraction of the calf muscle and is commonly linked with racquet sports (Squash, Badminton, Tennis) but can occur as a result of a fall or stumble. It can occur at any age but is most common in people between the ages of 30 and 50.
Causes:-
- Any muscle or tendon in the body can be torn if there is excessive stress placed on it.
- High impact sports, football, running, basketball, diving and tennis.
- Falls forcing the foot upwards and stretching & tearing the tendon.
- A deep cut in the tendon.
- Long-term use of Corticosteroids.
- Steroid injections near Achilles tendon.
- Cushing’s syndrome.
- A weak Achilles tendon from a previous sprain.
- Rheumatoid arthritis, gout and lupus.
Symptoms :-
- Comes on suddenly during a sporting activity or injury.
- You might hear a snap or feel a sudden sharp pain when the tendon is torn.
- The sharp pain usually settles quickly, although there may be some aching at the back of the lower leg.
- After the injury, the usual symptoms are :-
- A flat-footed type of walk.
- You can walk and bear weight but cannot push off the ground properly on the side where the tendon is ruptured.
- Unable to stand on tiptoe. If the tendon is completely torn, you may feel a gap just above the back of the heel.
- However, if there is bruising then the swelling may disguise the gap.
Diagnosis :-
Achilles tendon rupture is often misdiagnosed as a sprain, however an experienced Podiatrist will make a diagnosis from clinical examination and the history of the injury. A method known as the calf squeeze test may be used. The podiatrist will gently squeeze the muscle at the back of your leg and observe how the ankle moves (plantar flexion). This is an accurate test for Achilles Tendon Rupture.
Treatment :-
Non-surgical management traditionally was selected for minor ruptures, less active patients, and those with medical conditions that prevent them from undergoing surgery.
Low level laser therapy is effective in reducing the pain and inflammation and will accelerate the healing and help prevent the formation of scar tissue. None operative treatment is associated with a higher re-rupture rate however this is less invasive and the patient is less likely to suffer side effects and complications than more invasive methods.
If conservative methods fail surgery may be required. The period of immobilisation after surgery is about eight weeks and it takes about six months to return to normal activity. Treatment involves wearing a plaster cast or brace (orthosis) for several weeks, and possibly having an operation. Recent studies have produced superior results with much more rapid rehabilitation in fixed or hinged boots.
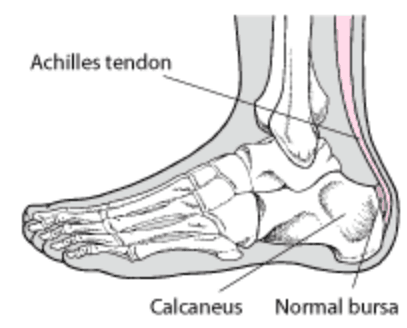
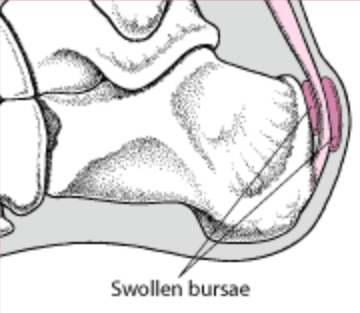
Bursitis is inflammation of the bursa which are small sacs of synovial fluid situated between the bones, tendons and joints. They act as buffers to protect these structures from friction and damage during movement. If a particular body part becomes injured or an infection has developed it can cause inflammation and pain of the affected bursa. The heels are often affected by bursitis.
There are three main types of Bursitis :-
Posterior Achilles tendon bursitis
Occurs mainly in young women who have Haglund’s deformity or ‘pump bumps’ but can develop in men. Walking in high heels or pumps that repeatedly press the soft tissue behind the heel against a stiff shoe counter can cause or aggravate this type pf bursitis.
Posterior Achilles tendon bursitis in the early stage may include redness, pain, and warmth at the back of the heel. If the damage continues the top layer of skin may wear away. After several months, a bursa appears as a soft tender inflamed, red or flesh-coloured nodule. In chronic cases the bursa may become hard like a scar.
Symptoms feel worse when walking, running, standing on tip toes, flexing the foot upwards or when the area is touched.
Retrocalcaneal bursitis
Anterior or deep to the achilles tendon is the retrocalcaneal bursa which may become swollen by any condition that puts extra strain on the Achilles tendon. Injuries to the heel, due to those caused by stiff or poorly fitting shoes and diseases such as rheumatoid arthritis and gout.
Wearing shoes and walking become difficult. A slightly red, swollen tender spot develops on the back of the heel. When the inflamed bursa enlarges, the swelling spreads sideways to both sides of the heel.
Policemans Heel
Policeman’s Heel refers to a protective sack of fluid, know as a bursa, which can form under the plantar tubercle of the heel bone. It is far less common that plantar fasciitis and usually occurs in people with a poor plantar fat pad on the heel.
It is often confused with plantar fasciitis but is not the same. The pain is situated in the middle of the heel pad and is caused by excessive friction and pressure during activity.
Causes :-
- Starting a very intense workout schedule.
- Suddenly increasing activity level without the right conditioning or footwear.
Treatment :-
- Avoid activities that cause pain.
- Warm or cold compress on the heel several times a day.
- Non-steroidal anti-inflammatory medications.
- Protective paddingInsoles/orthotics.
- Low level laser therapy.
- Stretching excercises to improve flexibility and strength around the ankle.
If associated with Achilles tendinitis, you may need to wear a cast on the ankle for several weeks.
Prevention :-
- Wear correct footwear when exercising & walking.
- Exercises to Maintain as good flexibility and strength around the ankle.
If these treatments are not effective, part of the heel bone may need to be surgically removed.
Low Level Laser Therapy has been shown to be very effective in treating this condition reducing the need for pain killing drugs.

Haglands bumps are bony enlargements on the posterior aspect of the heel. It is more common in women than men, or in those that have rear foot varus. It is not always painful but can be unsightly. If the bony enlargement is rubbed by foot wear or injured, a small fluid filled sac called a bursa becomes inflamed and a condition called bursitis develops.
Posterior Achilles bursitis is painful and can make walking and wearing certain foot wear difficult. They can appear on one or both feet.
Diagnosis is normally from clinical examination. The Podiatrist is able to assess the factors involved in order to prescribe the necessary corrections to assist recovery.
Causes:-
Haglund’s bumps are genetic but may be also aggravated by the gait of the person who tend to walk on the outer side of the heel.
Signs And Symptoms :-
Pump bumps appear as a noticeable bump on the back of the heel around the Achilles tendon. Swelling and redness may be seen in those who are suffering with pain and this will increase as the inflammation develops and the area becomes more warm and sensitive to the touch.
Treatment :-
- Resting
- Wearing open backed foot wear
- Cold compress several times a day
- Non-steroidal anti inflammatories
- Low level laser therapy
- Padding
- Orthotics to improve gait
- Foot wear wth soft backs
- Shoe modifications
Initially the condition may be treated conservatively as this is less invasive and means the person is less likely to suffer side effects and complications of invasive methods.
Pain relief, rest and ice application may help to reduce the discomfort, redness and swelling of the area which may be enough to ease the condition during flare-ups. Stretching exercises for the Achilles tendon to relieve the pressure of the tissues on the bony structures which in some cases may be sufficient to solve the problem.
For those who have not had any success with less invasive methods or those whose bump protrudes quite significantly surgery may be recommended. Once the surgical correction has taken place the Podiatrist can deal with the Biomechanics to prevent recurrence.
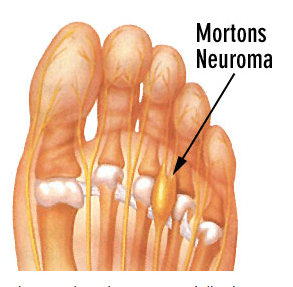
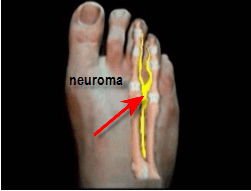
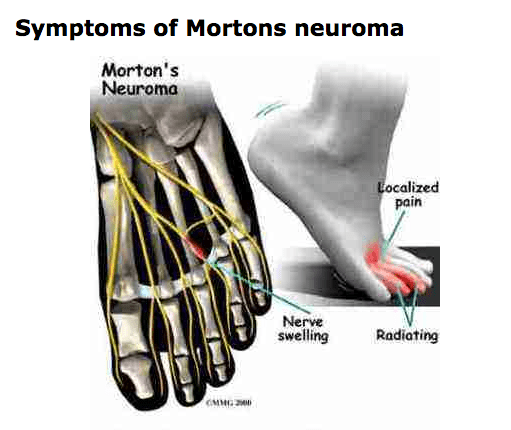
Morton’s Neuroma is an enlarged nerve causing pain in the forefoot normally between the third and fourth metatarsal heads. Forefoot problems may be caused by tight footwear, sports activities, walking. Foot deformities such as bunions, hammer toes and flat feet are amongst the causes.
Neuroma’s are very painful and people who have them may experience tingling, burning sensation, pain in the toes and forefoot. It can be described as just like walking on a stone and in severe cases numbness.
Also diagnosed by palpating the painful area on the forefoot and obtaining a ‘Mulder’s click’, this reproduces the symptoms. Examination of the painful foot during stance sometimes pushes the affected toes apart and this is called ‘Churchill’s sign’.
Treatments available for Morton's Neuroma
- Footwear-Identifying the shoes that sets off the pain and no longer wearing them may eradicate the problem.
- Anti-inflammatory medication for temporary relief only. There are potential systemic problems with taking this type of medication for long periods of time.
- Low Level Laser Therapy – for pain relief and tissue repair acts locally and may be used instead of taking oral anti-inflammatories. It is very gentle and effective in the treatment of Morton’s neuroma.
- Orthotics- A podiatrist may recommend a biomechanical examination. This evaluation is used to fabricate orthotic devices custom made to the structure of the patient’s foot. This controls abnormal structural components of the foot contributing to the condition and relieving pressure on the forefoot.
- Simple Insoles- Metatarsal pads can be build into the orthotic or simple insole which attempts to spread apart the adjacent metatarsal bones removing the pressure on the nerve, thus reducing pain. This type of Morton’s neuroma treatment is for patients who are not able to have other types of treatment and is the most conservative type available for this condition.
- ‘Chair side orthotics’ are a less expensive option than prescription orthotics for neuroma pain.
- Cortisone injection of the area may also help reduce the pain and swelling.
- Cryosurgery- A nonsurgical option that has become available in recent years is the use of cryosurgery under local anaesthesia. The neuroma is frozen by inserting a probe under the guidance of an ultrasonic scan which deadens the nerve thus eliminating the pain.
- Surgical removal of neuroma under local or general anaesthesia cuts the nerve out but may leave a permanent scar in its place called a ‘nubbin’which may be just as painful as the neuroma.
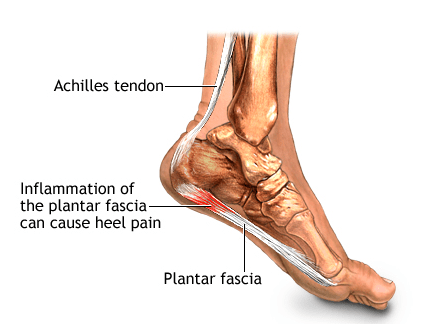
Plantar fasciitis is the most common cause of heel pain. Approximately 2 million patients are treated for this condition every year. It occurs when the strong band of tissue that supports the arch of your foot becomes irritated and inflamed. The plantar fascia is a long, thin ligament that connects the heel to the front of your foot.
Plantar Faciitis can be very painful and can be felt as a dull ache with episodes of a sharp pain in the heel or under the arch. The pain is often worse in the morning or after periods of rest and improves during the day.
Causes :-
The plantar fascia is designed to absorb the high stresses and strains we place on our feet. But, sometimes, too much pressure damages or tears the tissues. The body’s natural response to injury is inflammation, which results in heel pain and stiffness of plantar fasciitis.
In most cases, plantar fasciitis develops without a specific, identifiable reason. There are, however, many factors that can make you more prone to the condition:
- Tight calf muscles that make it difficult to flex your foot
- Weight gain
- Flat feet
- Very high arch
- Repetitive impact activity (running/sports)
- New or increased activity
- Footwear
- Injury
Heel Spurs
Although many people with plantar fasciitis have heel spurs, spurs are not the cause of plantar fasciitis pain.
One in 10 people may have heel spurs, but only 1 in 20 people with heel spurs have foot pain. Because the spur is not the cause of plantar fasciitis, the pain can be treated without removing the spur.

X-ray of heel spur
Diagnosis is normally from patient history and clinical examination, the Podiatrist will discuss the best course of action to relieve symptoms.
Nonsurgical Treatment
Primarily we treat this condition conservatively as this is less invasive and the patient is less likely to suffer side effects and complications than more invasive methods.
90% of patients may improve within 10 months of starting simple treatment methods.
Rest
Decreasing or even stopping the activities that make the pain worse is the first step in reducing the pain. You may need to stop athletic activities where your feet pound on hard surfaces (for example, running or step aerobics).
Ice
Rolling your foot over a cold water bottle or ice for 20 minutes is effective. This can be done 3 to 4 times a day.
Oral Medication
Non-steroidal anti-inflammatory medication such as ibuprofen or naproxen reduce pain and inflammation.
Exercise
Plantar fasciitis is aggravated by tight muscles in your feet and calves. Stretching your calves and plantar fascia is an effective way to relieve the pain.
Orthotics
A biomechanical assessment will provide both static and dynamic information which is then used to fabricate custom made orthotics this will relieve the stress on the plantar fascia.
Low Level Laser
Low level laser therapy is effective in reducing the pain and inflammation and will accelerate the healing. With its ability to reduce inflammation and ease pain, laser therapy achieves good results in the treatment of plantar fasciitis where it stimulates the fibroblasts for a faster regeneration of connective tissue structures in the tendon. Treatment generally involves direct application to the heel with an infra-red probe to be repeated every 2-3 days for 2-3 weeks.
Other treatments may include night splints or a steriod injection.
For more information click here
Severs disease is a condition that causes heel pain and affects children and young adults between the ages of 10-18. Although more common in boys as they tend to have later growth spurts it also happens to girls at an earlier age. Nearly always associated with activity particularly running and jumping as a result it places the Achilles tendon under enormous stress causing muscle fatigue.
Causes :-
During a child’s growth spurt the soft tissues are unable to keep up with bone growth causing the muscles, tendons and ligaments at the back of the heel to become tight furthermore the heel is one of the first bones in the body to reach full adult size. The Achilles tendon pulls the bone away from the maturing growth plate during high impact activity causing heel pain.
Symptoms :-
- Pain, swelling & redness in one or both heels
- Tightness & tenderness in the back of the heel – feels worse when squeezed.
- Heel pain increases after running or jumping and feels better after rest
- Difficulty walking
- Walking or running with a limp or on tip toes
The condition can be very disruptive to an individuals quality of life. Sever’s does not cause any long-term foot problems. Symptoms disappear after a few months.
Treatments :-
- Resting or reducing the activity until the pain improves then reintroducing the sports gradually.
- Ice packs
- Stretching exercises
- In severe cases may need a cast so that the heel is forced to rest.
- It can be effectively treated by low level laser therapy, orthotics & advise on appropriate footwear.
Prevention :-
- Supportive shoes
- Stretching exercises
- Warn against over training
- Avoid lots of running on hard surfaces
- Avoid gaining too much weight